Foot & Ankle Pain
What is an Ankle Sprain?
Excessive motion in the ankle is prevented by the stabilisation of the ankle joint, which is provided by ligaments. When these ligaments are given excessive flexion; beyond the range they move naturally, the movement of the ankle will deviate from the regular joint movement.
Sprains often occur due to a specific direction of force, affecting the three primary outer ankle ligaments. These ligaments can stretch or tear, and in severe cases, this can lead to fractures, other injuries, or joint displacement.
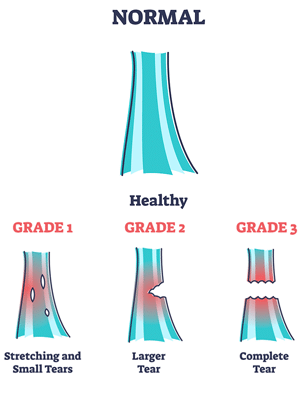
Depending on the damage caused to the ligaments, ankle sprains have three different categories:
- Grade 1: The ligament is partially torn.
- Grade 2: The ligament is incompletely torn and there is moderate loss of function.
- Grade 3: The ligament is completely torn and its integrity lost.

Treatment for Ankle Sprain
Depending on the grade of ligamentous injury, there are various treatments.
Grade 1 injuries need rest, ice, compression, and elevation. Limiting activity and non-steroidal anti-inflammatory medicines can help.
PBM Laser therapy and support braces will greatly reduce inflammation and speed up the healing process.
For Grade 2, in addition to what is used in grade 1, prolotherapy injections will boost the bodies self healing properties.
With Grade 3 injuries, Autologous Conditioned Plasma Injections are the recommended treatment course. These injections will greatly boost the bodies self healing properties. In some cases, they are required to restart the bodies healing process.
What is Plantar Fasciitis?
Plantar fasciitis is a painful inflammatory heel condition that affects the large ligament-type structure in the base of the bottom of the feet. Some may develop plantar fasciitis as a result of wear and tear over certain physical activities or ill-fitted shoes.
The plantar fascia can become thick and inflamed due to the irritation at its attachment, at the base of the heel. Some doctors may say heel spur is the underlying diagnosis of plantar fasciitis. However, this diagnosis is misleading as the spur itself does not cause pain. Instead, the source of pain is the inflammation within the plantar fascia surrounding the bone spur/ heel spur itself. Heel pain is common, first thing in the morning when you are climbing out of bed and/or after periods of rest.
The plantar fasciitis pain can be inconsistent. Often there are pain-free periods when the you feel like they are healed, only for it to suddenly come back.
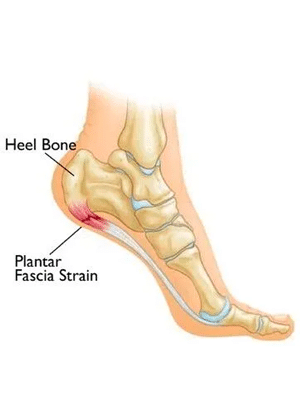
On the other hand, plantar fascia tearing pain is sharp and consistent.
It is important that your clinician differentiates between regular plantar fasciitis and plantar fascia tearing as the treatment is completely different. Here at the Foot, Ankle & Body Experts Health Clinic, we use diagnostic ultrasound imaging correctly identify and diagnose your condition.
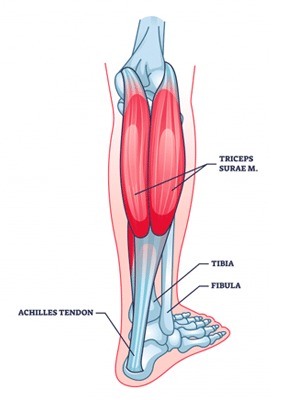
What is Achilles Tendonitis?
Achilles tendonitis refers to the inflammation of the Achilles tendon, the body’s largest tendon, which interestingly receives the least oxygen. This limited blood supply to the Achilles tendon renders it vulnerable to injuries, particularly in activities that involve jumping or sprinting.
As a result, individuals who heavily rely on their calf muscles, such as ballerinas, basketball players, football players, and AFL players, are frequently affected by this condition.
Treatment for Achilles Tendonitis
While not always requiring surgery, the tendon is slow to heal, often taking a number of months. The approach to treating Achilles tendonitis aims at reducing inflammation, pain, and promoting the tendon’s healing.
The treatment varies based on the severity of pain and the duration of the condition. At our clinic, we offer a comprehensive set of options, such as:
What is Metatarsalgia?
Metatarsalgia refers to pain and inflammation in the ball of the foot, specifically in the area of the metatarsal bones, which are the long bones in the foot that connect to the toes. This condition is commonly experienced as a sharp, aching, or burning pain in the ball of the foot, and it can be aggravated by standing, walking, or running.
What causes Metatarsalgia?
- Overuse: Repetitive activities or high-impact sports can put excessive pressure on the metatarsals.
- Foot Shape: A high arch or a prominent metatarsal head can contribute.
- Excess Weight: Carrying extra weight can put added stress on the metatarsals.
- Improper Footwear: Shoes that are too tight, too narrow, or with high heels can exacerbate pressure on the ball of the foot.
- Hammertoe: Misalignment of the toes can shift weight distribution.
- Bunions: These can change the way weight is distributed across the foot.
- Stress Fractures: Small breaks in the metatarsals can be painful and increase pressure.
- Morton’s Neuroma: Thickening of the tissue around a nerve can cause similar symptoms.
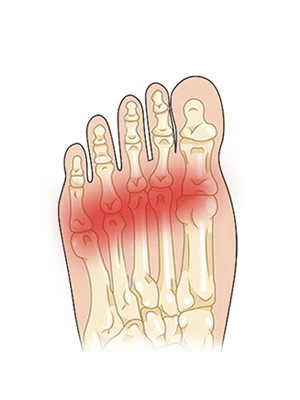
What are the symptoms?
- Sharp, aching, or burning pain in the ball of the foot.
- Aggravation of pain during weight-bearing activities.
- Tingling or numbness in the toes.
- A feeling of having a pebble in your shoe.
It’s crucial to see a healthcare professional if you suspect you have metatarsalgia, as proper diagnosis and treatment can help alleviate the pain and address the underlying causes.
What is Morton’s Neuroma?
Morton’s Neuroma is a foot condition characterised by a thickening of the tissue around one of the nerves leading to the toes. This can cause a sharp, burning pain in the ball of the foot or a feeling as if one is standing on a pebble in their shoe or on a fold in their sock. The pain may also radiate out to the nearby toes. Typically, Morton’s neuroma occurs between the third and fourth toes, but it can occur between other toes as well.
What causes Morton’s Neuroma?
- Footwear: High heels or shoes with a tight toe box can compress the toes, increasing the risk of Morton’s neuroma.
- Repetitive Strain: Activities that put repetitive pressure on the ball of the foot, like jogging or dancing, can contribute.
- Foot Deformities: Bunions, hammertoes, high arches, or flat feet can predispose an individual to Morton’s neuroma
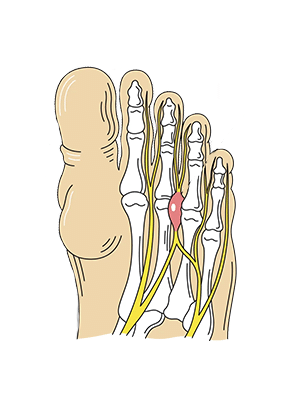
The symptoms Morton’s Neuroma?
- Pain in the ball of the foot.
- Tingling, burning, or numbness in the toes.
- A sensation as if standing on something inside the shoe.
- Pain that increases with activity or wearing shoes.
What causes flat feet? Is it an issue for me?
Flat feet, also known as fallen arches or pes planus, is a condition where the arches of the feet collapse or are very low, allowing the entire sole of the foot to come into complete or near-complete contact with the ground. While many people with flat feet experience no issues, some might encounter pain or other problems.
- Genetics: Inherited foot structures can predispose an individual to flat feet.
- Foot or Ankle Injuries: Trauma can damage the structure and function of the foot.
- Rheumatoid Arthritis: This inflammatory condition can cause flat feet.
- Muscle Diseases: Conditions like cerebral palsy or muscular dystrophy can lead to flat feet.
- Aging: The tendons in the feet can weaken over time, leading to fallen arches.
- Pregnancy: Hormonal changes combined with the weight and pressure of pregnancy can flatten arches.
- Obesity: Excess weight can put additional strain on the foot, leading to flat feet.
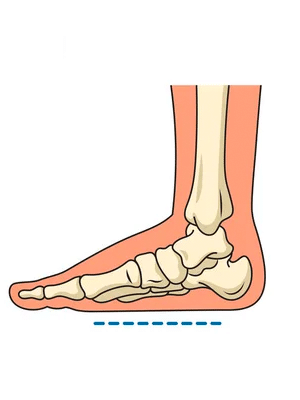
Flat Feet Symptoms?
- Feet that tire easily or become painful with prolonged standing or walking.
- Pain in the arches or heels.
- Back or leg pain.
- Inside ankle swelling.
- Feet that point outward when relaxed.
What is Diabetic Foot?
Diabetic foot refers to the foot-related complications that arise as a consequence of diabetes mellitus. Diabetes can damage both the circulatory and nervous systems, which plays a critical role in the health of one’s feet. Here’s a breakdown:
Effects on the Circulatory System
- Reduced Blood Flow: The extremities, particularly the feet, receive decreased blood circulation due to the narrowing or hardening of arteries. This reduced blood flow can delay wound healing and increase the risk of infections.
- Poor Oxygenation and Nutrient Supply: With compromised circulation, the feet get less oxygen and fewer nutrients, which are vital for tissue repair and general health.
Effects on the Nervous System
- Peripheral Neuropathy: Diabetes can cause nerve damage, particularly in the feet. This means patients might not feel pain, heat, or cold in their feet, which increases the risk of unnoticed injuries.
- Changed Foot Shape: Due to muscle weakness and foot deformities that can arise from nerve damage, the foot might change shape, leading to areas of increased pressure and potential ulceration.

Potential Foot Problems in Diabetics
- Foot Ulcers: Open sores that can develop due to unnoticed injuries, pressure points, or poor circulation.
- Infections: Reduced sensation and poor blood flow make diabetics more susceptible to severe foot infections.
- Cellulitis: An acute spreading bacterial infection within the skin’s deeper layers and possibly into the bloodstream.
- Charcot Foot: A condition characterised by swelling, redness, and joint dislocation due to nerve damage.
- Dry and Cracked Skin: Can become entry points for bacteria leading to infections.