By Dr YeJeong Kim
Understanding Achilles Pain: From Tendinitis to Tear
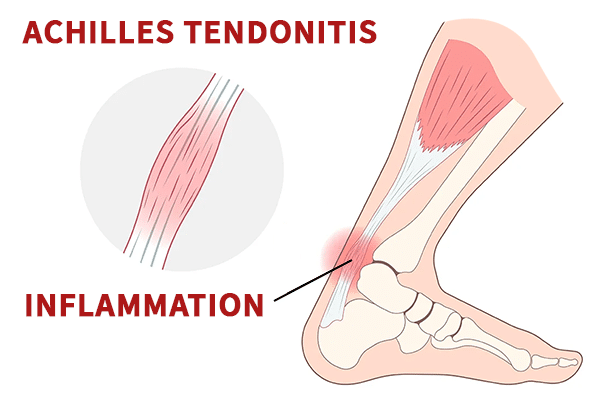
The Achilles tendon is the strongest tendon in the human body. It connects the calf muscles to the heel bone and plays a crucial role in walking, running, and jumping. Normally about the thickness of two fingers (approximately 4 to 6 mm), it absorbs a tremendous amount of force with every step—especially during high-impact activity.
However, with repeated stress or overuse, the tendon can become irritated and inflamed—a condition known as Achilles tendinitis. When this happens, the tendon may thicken significantly, sometimes doubling in size, particularly a few centimetres above the heel where pain is most commonly felt. Achilles tendinitis is especially common in runners, with up to 10–20% experiencing symptoms at some point in their training.
Common Symptoms
Typical signs of Achilles tendinitis include pain and swelling along the tendon, usually 3 to 5 centimetres above the heel. The area may feel warm or tender to the touch. Stiffness is often worse in the morning or after periods of rest. In more severe cases, walking may become difficult, and a limp can develop.
How Is It Diagnosed?
I begin with a thorough physical examination to assess the Achilles tendon and surrounding structures. In most cases, this gives me a clear indication of the issue. To confirm the diagnosis and better understand the extent of inflammation or injury, I also perform in-room diagnostic ultrasound during the consultation.
Ultrasound allows me to visualise changes such as tendon thickening, irritation, or small tears, and I can assess how the tendon moves and responds in real time. If the condition is complex or requires further evaluation, I may refer for an MRI scan to gain additional detail.
Treatment and Recovery
When treating Achilles issues, my approach depends on whether the tendon is simply inflamed or if a tear has occurred.
If the tendon is irritated or thickened but not torn — as in tendinopathy — we focus on reducing load and supporting healing through conservative care. This might involve modifying training routines, shortening running distances, and shifting to low-impact activities. I often recommend supportive footwear, including a small heel lift or rocker-bottom sole, to reduce strain on the tendon during daily movement. Anti-inflammatory medication can provide short-term relief, though I avoid steroid injections, as they carry a risk of weakening the tendon.
For more persistent symptoms, I use in-clinic shockwave therapy, which has shown excellent outcomes for chronic Achilles tendinopathy. I also offer regenerative treatments such as prolotherapy and platelet-rich plasma (P.R.P) injections, which are particularly helpful for cases that haven’t responded to conventional care.
If there’s a partial tear, treatment depends on the severity. In some cases, a period of offloading in a boot, combined with regenerative injections and structured rehabilitation, can allow the tendon to heal without surgery.
However, if the tendon has ruptured completely — which usually presents with a sudden pop, followed by weakness or an inability to push off the foot — surgical repair is often required. After surgery, rehabilitation is essential to restore strength, flexibility, and function, and to reduce the risk of future injury.
Achilles tendinitis is manageable, especially when addressed early. If you’re noticing persistent heel or ankle pain, don’t wait for it to become a long-term issue. Getting the right diagnosis and treatment early can prevent further damage and help you recover faster.


